Optum Review: St. Louis County Medicaid Problems From Policy Weaknesses, Not Fraud
Optum found policy and system weaknesses in Minnesota Medicaid billing—not proof of fraud—highlighting risks that could affect local Medicaid services and payments.
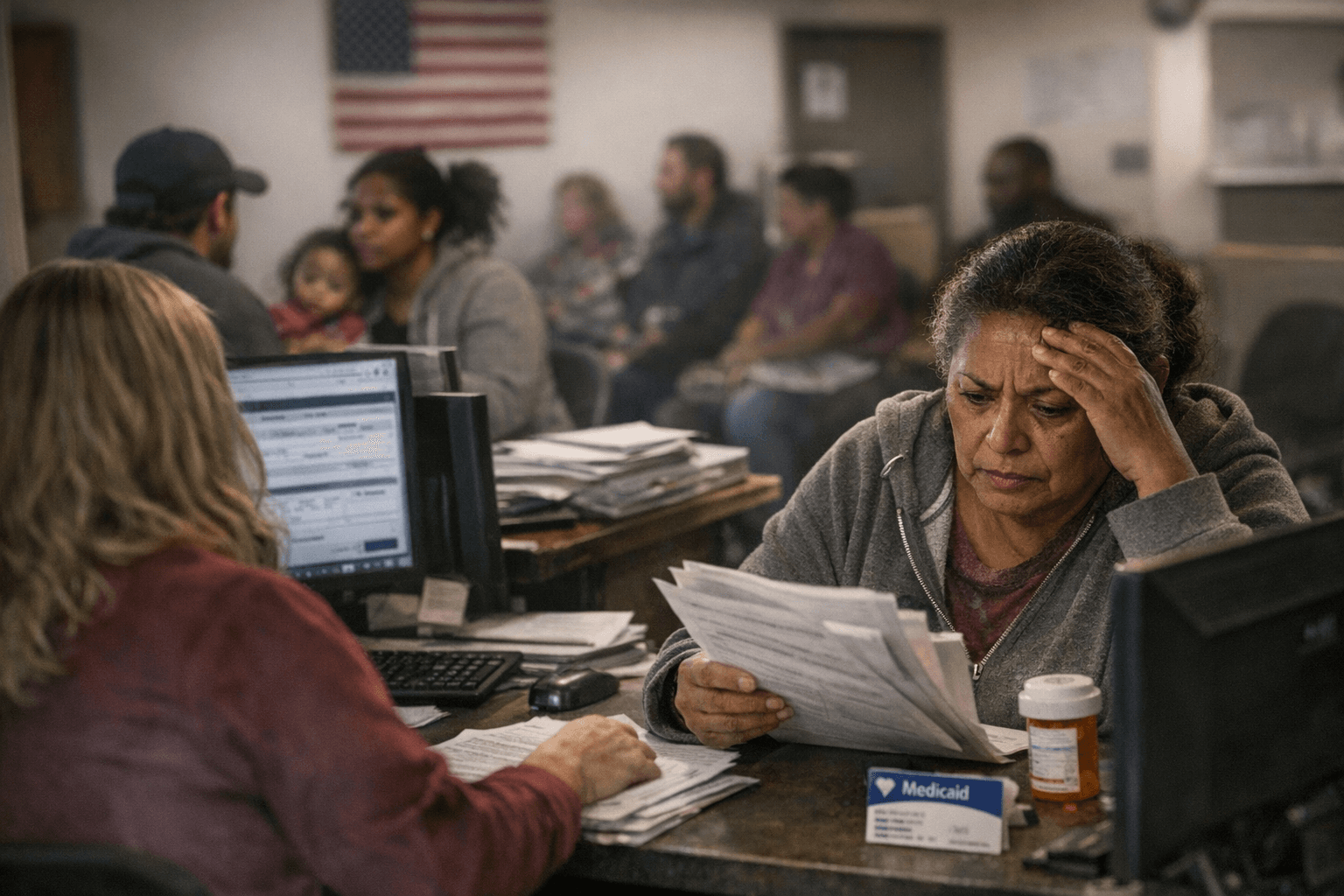
An Optum vulnerability assessment of Minnesota’s fee-for-service Medicaid billing found widespread policy and system weaknesses that created millions in recoverable payments and billions in dollars at risk, but stopped short of calling the issues fraud. The findings matter for St. Louis County residents who rely on Medicaid services and providers that bill the program.
The review examined roughly 20 percent of the state’s Medicaid billing across 14 programs the Minnesota Department of Human Services designated as high risk, covering January 2022 through October 2025, a 46-month period. Optum identified $52.3 million in what it terms direct recoveries - payments tied to clear policy violations that the state could seek to claw back under existing rules. Non-Emergency Medical Transportation accounted for about $24 million of those payouts, and the report flags Early Intensive Developmental and Behavioral Intervention, individualized home supports, and night supervision among the largest contributors.
Beyond direct recoveries, Optum estimated $1.7 billion in potential improper payments over the same 46-month window. Another estimate in the assessment and related briefings placed the preventable-savings figure at $1.75 billion, with autism services alone accounting for just over $1 billion of that total. Optum emphasized its findings highlight “potential program integrity risk and operational vulnerabilities” and are “not determinations of waste, fraud and abuse.”
Optum traced the problems to vague rules, policy loopholes, failures of automatic system edits, and recurring vulnerabilities that “stemmed from weakness in monitoring, auditing and inter-agency communication.” In a press call, Connolly said “an example of this may have been providers filing claims improperly.” The Minnesota Department of Human Services told reporters: “In the interest of transparency, we shared the information in the report as soon as it was available for release, but that also means we need more time to review its results.” DHS also said it will “continue to refine work on the pre-payment system,” and that any suspicious activity will be referred to law enforcement; Optum said further studies will be conducted over the next nine months.
Federal context underlines that many audit findings reflect compliance and control failures rather than intentional schemes. The Government Accountability Office reported that 69 percent of Medicaid single audit findings in fiscal years 2019–2021 involved noncompliance and 36 percent were material weaknesses. CMS guidance on investigations notes program integrity contractors generally open cases where exposure exceeds $50,000, while single audits are required when federal award expenditures meet or exceed $750,000.
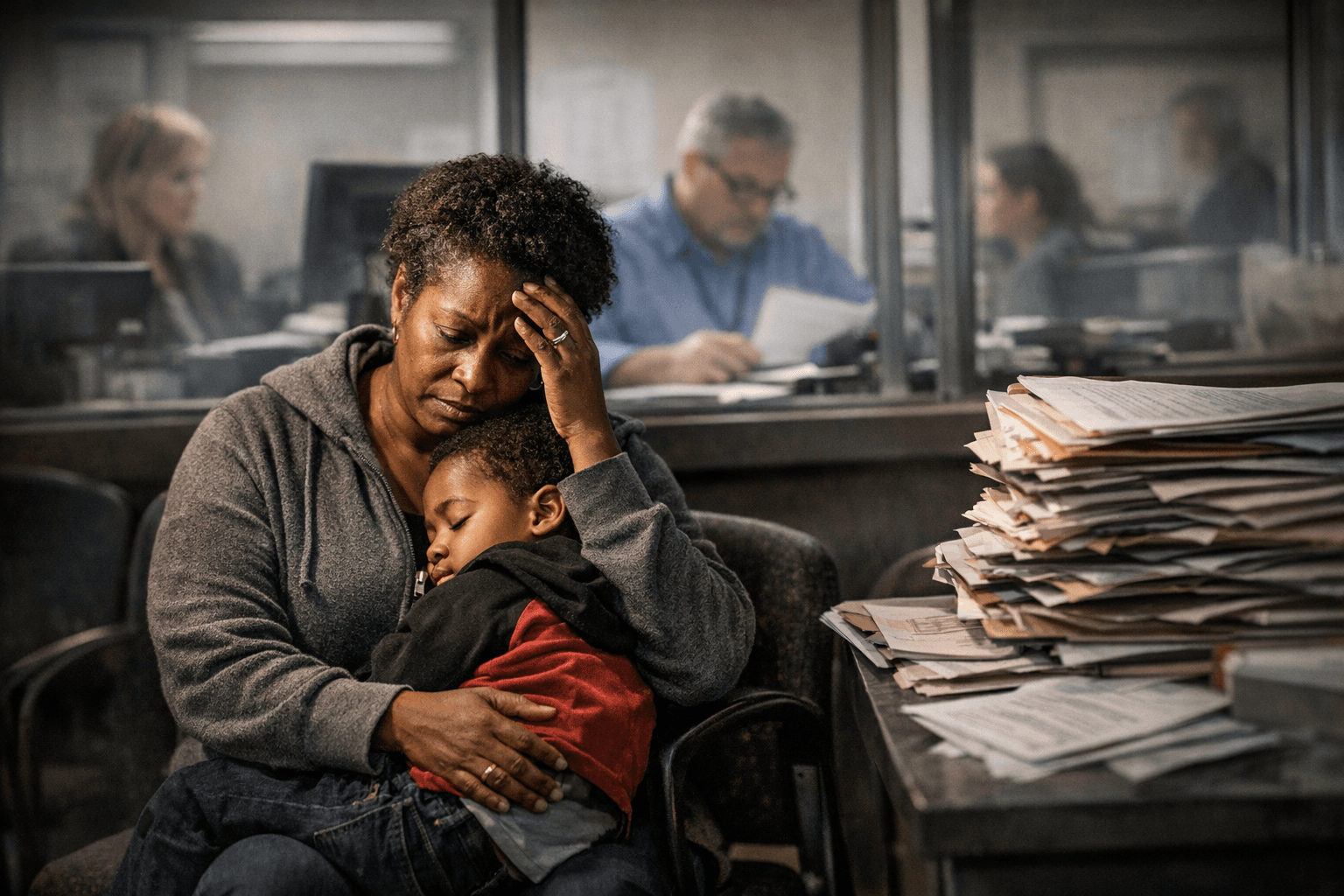
For St. Louis County, the review signals that policy fixes and better pre-payment checks could protect Medicaid dollars and reduce billing errors that affect local providers and patients. Expect state follow-up work in coming months and possible targeted audits; families using autism services, NEMT, and home supports should watch for communications from providers or DHS about billing or program changes as officials refine controls and investigations proceed.
Sources:
Know something we missed? Have a correction or additional information?
Submit a Tip

